Antibiotic Resistance: A Food Safety Issue
Due to misuse of antibiotics, many harmful bacteria have mutated in such a way that they are no longer susceptible to antibiotics. Antimicrobial resistance has lead to a steep increase of death rates from certain infections, such as methicillin-resistant Staphylococcus aureus (MRSA). This ‘silent epidemic’ already affects hundreds of thousands of Americans. MRSA alone causes tens of thousands of deaths each year in the U.S. Often, the burden of antibiotic resistance is borne by the most vulnerable in our society: children, the elderly and those with already weakened immune systems, such as people undergoing chemotherapy.
Antibiotic-resistant Foodborne Pathogens
MRSA and vancomycin-resistant Enterococcus faecium are examples of antibiotic resistant bacteria that cause serious problems in hospitals today. These resistant foodborne pathogens should not be neglected. Various outbreaks of antibiotic-resistant Salmonella strains (Heidelberg, Typhimurium, Newport and Hadar), originating from ground beef, ground turkey or turkey burgers, have been reported in the U.S. in recent years. Outbreaks were also caused by several resistant serotypes of enterotoxigenic Escherichia coli (ETEC) and resistant Campylobacter jejuni.
A sharp increase of antibiotic resistant foodborne pathogens has been reported. U.S. Centers for Disease Control and Prevention (CDC) data show that roughly one in five Salmonella infections is now drug-resistant. Nearly 100,000 of these infections resist treatment with at least five antibiotics. Roughly one-half of Campylobacter infections, or 1.2 million per year, are drug-resistant. Of these, 326,000 cases are resistant to two or more antibiotics. Antibiotic resistant strains of Listeria monocytogenes have been detected as well.
Overuse of Antibiotics Likely to be Restrained
The overuse of antibiotics occurs in both human medicine and animal agriculture. CDC reports that approximately 50 percent of antimicrobials, particularly antibiotics, were unnecessarily or inappropriately prescribed in U.S. hospitals and doctors’ offices. In response, the World Health Organization and many national authorities are now urgently calling for a cut in the use of antibiotics. Doctors have started to curtail the use of antibiotics in human health to slow down the emergence of antibiotic resistance.
However, according to an U.S. Food and Drug Admnistration (FDA) estimate, about 80 percent of all antibiotics sold in the US are used in animal agriculture. Notably, non-therapeutic usage represents a substantial portion (probably in the order of 70%) of all antibiotics used in livestock production.
Voluntary guidelines released by FDA promote the judicious use in food-producing animals of antibiotics that are important in treating humans. Furthermore, FDA recommends the use of medically important antimicrobial drugs in food-producing animals to be limited to situations where this is necessary for treating sick animals. Use of medically important antimicrobial drugs to increase animal production is not considered to be judicious. Recent rulings, filed in lawsuits brought by environmental and public health groups, highlight the potential for future—more stringent and compulsory—shifts in federal regulations over animal agriculture practices. Such changes could force beef, pork and poultry producers to restrict the use of antibiotics tremendously.
Phages: A Natural Alternative to Antibiotics
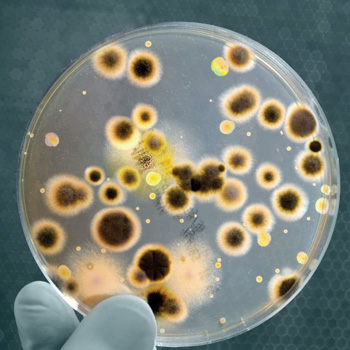
The preventive use of phages offers an important alternative to antibiotics in the current era of multidrug resistant pathogens. In nature, phages kill roughly one-half of all bacteria on our planet every 2 days. Phages have been applied successfully as bactericidal agents to treat human infections and in veterinary medicine.
Prophylactic use, for instance, in the area of livestock produce or food production and processing, can help push back the use of antibiotics without compromising food safety. This includes pre-slaughter interventions at farms by adding phages directly to animal feed or drinking water. However, application of phages as clean label processing aids in food production and preparation areas can also help ensure food safety. Use of phages does not affect the susceptibility of bacteria to antibiotics.
Phage products show bacteriocidal effects that can be measured within hours. They withstand a wide range of food processing conditions, do not affect organoleptic properties of the treated products, leave starter cultures unaffected and are non-corrosive. With phage products, cost effective applications ensuring food safety are within reach of every company.
The Downside of Antibiotics
Apart from resistance issues, there are other issues relating to today’s high use of antibiotics in many developed countries. Most bacteria on our skin and in our gut are actually good and help protect us. Antibiotics cannot distinguish between good and bad bacteria; they kill all bacteria, except those that are resistant. In addition, antibiotics are known to have many side effects, ranging from allergic reactions and diarrhea to fever, nausea and skin inflammation. This is why inappropriate use of antibiotics should be strongly discouraged.
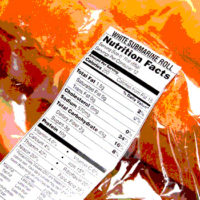
When it comes to food products, recent findings suggest that residual levels of antibiotics in fermented meat products like salami and pepperoni, pose a food safety threat by inhibiting microbial starter cultures and subsequent fermentation processes, allowing pathogens to multiply during processing. This overlooked risk associated with the presence of veterinary antibiotics in meat may prompt legislators to reconsider tolerable levels of residual antibiotics. Additional food safety measures by food processors with respect to these types of meat should be considered.
Phage Technology
Bacteriophages (phages)—Greek for ‘bacteria-eaters’—were discovered nearly a century ago. They are present in high numbers in our normal environment, including the human body, freshwater and marine habitats, the gastrointestinal tract of food animals and many foodstuffs. The unique property of phages lies in the fact that they attack specific bacteria and kill only those. Hence, specific phages can be used against only the ‘unwanted’ bacteria, that is, in human or veterinary medicine and in the production of food.
Micreos is a global player in the field of phage technology. In 2006, this Dutch company was the first to bring an FDA Generally Recognized as Safe-approved phage product to the market: LISTEX™, effective against a broad spectrum of the deadly Listeria monocytogenes. LISTEX™ is now used successfully by many manufacturers in the meat, cheese and fish industry. Micreos is currently testing its new product, SALMONELEX™, against Salmonella.
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!