Salmonella and Campylobacter: A Methods Update
Salmonella spp., Campylobacter jejuni and Campylobacter coli recognized as the leading causes of bacterial foodborne diarrheal disease. In the United States, Campylobacter species are isolated from about 5% of the patients with diarrhea and the annual incidence of infection is estimated to be 50 per 100,000 population, while salmonellosis is about 16 per 100,000 population. The good news is that, according to the latest figures on reductions in foodborne illness from the Centers for Disease Control and Prevention (CDC), both Salmonella and Campylobacter infections significantly declined from 1996 to 2003. These declines—Salmonella (17%), Campylobacter (28%) and Salmonella Typhimurium (38%)—are encouraging and credit is due to the food processing industry for its efforts in implementing science-based testing protocols and pathogen reduction intervention systems and technologies.
With regard to testing, the food industry has been continuously in search of rapid and cost-effective methods for enumerating and identifying microorganisms on food products and processing equipment to replace more time-consuming and labor-intensive conventional methods. Since many types of fresh products are shipped within a day of processing, the time required for microbiological evaluations to be completed becomes critical. For example, this is true of freshly processed poultry products, frequently associated as high-risk product for Salmonella and Campylobacter. These products should be shipped within 24 hours of processing, and certainly, waiting for test results in order to ship can have a tremendous negative impact on the processor’s ability to conduct business profitably. However, not waiting and having a sample test positive for pathogenic contamination can result in costly recalls, human pain and suffering, loss of reputation, and costs associated with litigation.
Thus, in order to ensure the safety and quality of the product upon release, food processors know the necessity for rapid evaluation. In this article, we’ll briefly review some of the current research, regulations and rapid and automated identification and detection methods available to processors for the evaluation of Salmonella and Campylobacter in food products.
Salmonella Methods
CDC estimates that 1.4 million illnesses occur each year in the U.S. from the more than 2,000 strains of Salmonella, with infections associated with this pathogen resulting in more than 16,000 hospitalizations and nearly 600 deaths. Half of salmonellosis cases are caused by two serotypes: S. Enteritidis (SE) and S. Typhimurium (ST). CDC estimated that 118,000 illnesses were caused by consumption of S. Enteritidis-contaminated eggs in 2001.
The most common food vehicles for non-typhoid Salmonella are poultry, meat, eggs, milk, and their products. Salmonella has also been detected in chocolate, peanuts, shellfish, and a wide range of produce, including alfalfa sprouts, artichokes, celery, cantaloupe, cauliflower, eggplant, endive, fennel, green onions, lettuce, orange juice, pepper, salad greens, spinach, strawberries, tomatoes and watermelon. Salmonella is often associated with chickens, and deservedly so to a point, but the Centers for Disease Control and Prevention (CDC) has not reported in a number of years the full gamut of outbreak sources. Chicken is only one of many potential sources. In terms of foodborne illness outbreaks linked to Salmonella in recent years, many have been associated with tomatoes, orange juice, cantaloupe, melons, beef and pork. Chicken, clearly, is an important part of that, but unlike Campylobacter where 50%-70% of cases are epidemiologically linked to chicken, chicken is associated with only 10%-20% of foodborne salmonellosis cases.
Regulation and Research. The usefulness of the methods reviewed here often are linked to regulation and guidance issued by federal food agencies, which may require testing, either of finished product or to verify that process controls are working. The Salmonella performance standard for meat and poultry products was mandated in the 1996 Pathogen Reduction and Hazard Analysis and Critical Control Point (HACCP) final rule is well established, for example. These are based on the nationwide average prevalence of Salmonella in raw meat and poultry products, as determined by the FSIS Nationwide Microbiological Baseline Data Collection Programs and FSIS Ground Product Microbiological Surveys. The NACMCF has been charged with reviewing an FSIS proposal to revise the Salmonella performance standards for meat and poultry products, particularly raw ground beef and broilers, to better reflect the industry’s current ability to control or reduce Salmonella prevalence in these products.
In the past several years, FDA has proposed and implemented rules and issued guidelines with respect to Salmonella contamination of product categories under its purview. Guidelines pertaining to the surveillence and testing of alfalfa sprouts, cantaloupe, raw milk and raspberries, for example, were issued by the agency following well-publicized outbreaks associated with the pathogen. In 2001, FDA issued the Juice HACCP rule, developed in response to a rise in the number of outbreaks associated with citrus juices at that time, including a Salmonella Enteritidis outbreak in 2000 caused by unpasteurized orange juice that resulted in 88 illnesses in six western states and a Salmonella Muenchen outbreak in 1999 caused by unpasteurized orange juice that resulted in 423 illness in 20 states and three Canadian provinces and contributed to one death. Under the mandate, processors must use controls or interventions that “achieve a 5-log reduction in the numbers of the most resistant pathogen in their finished products compared to levels that may be present in untreated juice. Citrus processors may opt to apply the 5-log pathogen reduction on the surface of the fruit, in combination with microbial testing to assure that this process is effective.”
In 2004, the agency moved forward on an action plan to minimize foodborne illness associated with fresh produce consumption, which targets the reduction of microbial food safety hazards such as Salmonella. Among the extensive list of intervention and surveillence objectives in the action plan is FDA’s plans to “develop additional sampling protocols, as needed, to facilitate efficient and reliable detection of pathogens in or on fresh produce and in the fresh produce production environment” and to “develop revised or new analytical methods for improving the timely detection of pathogens in or on fresh produce and in the fresh produce production environment, with a focus on the commodity/pathogen combinations of greatest public health concern.”
Very recently, FDA issued a proposed rule to reduce the incidence of Salmonella Enteritidis (SE) in shell eggs during production, which outlines a program of farm-to-fork preventive measures and requires some testing. Specifically, shell egg producers would perform environmental testing for SE in poultry houses and in the event of a positive sample, further testing would be required and positive eggs would be held from entering commerce. According to the agency, producers would have to “conduct environmental testing for SE as an indicator of whether SE prevention measures are working effectively, if:
• They have 3,000 or more laying hens that produce shell eggs for the table market,
• They do not sell all their eggs directly to consumers, and,
• Any of their eggs that are produced at a particular farm do not receive a treatment that achieves at least a 5-log destruction of SE or are processed into egg products.
 Methods. There are several rapid and automated microbiological techniques available to food processors for the identification and detection of Salmonella in food products (Table 1). Those widely used include miniaturized biochemical, immunoassay, impedance/conductance, immuno-latex agglutination and DNA based methods.
Methods. There are several rapid and automated microbiological techniques available to food processors for the identification and detection of Salmonella in food products (Table 1). Those widely used include miniaturized biochemical, immunoassay, impedance/conductance, immuno-latex agglutination and DNA based methods.
Biochemical Methods. Considered a gold standard technique since an inexpensive miniaturized method for identifying bacterial isolates was developed by Fung in 1969, this technique involves the use of a 96-well microtitration plate in which microbiological growth media containing specific biochemicals are placed. A number of biochemical identification kits have been developed as a means of rapidly identifying certain groups of bacteria. To use these kits, bacteria are suspended in saline and a strip containing various biochemical assimilation tests is inoculated with the suspension. The strip is incubated for a specified period of time at a specific temperature. After incubation, the biochemical reactions are determined either manually or the strips may be read automatically. Some biochemical reactions require additional reagents to be interpreted. The biochemical reactions are used to obtain a number. By comparing the number to a database, the bacteria are identified.
Overall, when compared to conventional methodology, these miniaturized biochemical techniques for identification of bacteria are accurate, require less incubator space, require no time, labor, or materials for preparation, and results can be obtained much more rapidly. Also, the consistency of the materials used in these kits is very good. Errors associated with improper sterilization or preparation of media are avoided with these kits. However, these miniature kits are subject to inoculation error because a specified bacterial concentration must be used in the suspension or the results will not be accurate.
Immunoassay. Immunoassay is based on the qualitative or quantitative determination of antigen or antibody present in a sample by specific antigen-antibody reaction, which can be visualized in terms of clumping or agglutination, color or fluorescent development from an enzyme reaction or formation of an immunoband. The development of monoclonal antibodies directed against specific antigenic fractions of targeted microorganisms has led to the application of a number of immunological techniques in the food industry.
Polyclonal enzyme immunassay (EIA) and enzyme-linked immunosorbent assay (ELISA) procedures have gained much popularity in the last decade as a means of detecting specific populations of pathogenic bacteria. EIA and ELISA assays are quite sensitive and specific, although it should be noted that some food matrices may inhibit these tests. The use of ELISA assays can shorten the time for analysis by screening out negative samples and identifying presumptive positives for further analysis. Test formats for these assays include portable, self-contained dipsticks, test strips and vials in kit form, and automated benchtop systems. Many immunoassay tests can be cost-effectively performed in less than 24 hours, and automated immunoassay systems provide the ability to test many samples simultaneously.
Other rapid immunological techniques employed in the identification and detection of Salmonella include lateral flow assay, immunomagnetic separation and chromogenic media. Lateral flow assay is an antibody-antigen sandwich complex that detects microorganisms of interest based on liquid capillary action moving up a strip. After enrichment, the sample flows up the membrane by a wicking action through through an area containing colored particles coated with a specific antibody. If the antigens are present, they bind to the colored particle antibody conjugate, forming an antibody-antigen complex, which migrates through a nitrocellulose membrane. If, after passing through the next immobilized antibody zone, the antigen is present, the complex is captured and visualized by the formation of a colored line. Detection times can be a little as 10 minutes, and total test time depends on the enrichment method and detection limit required.
The use of immunomagnetic separation (IMS), once considered novel, is becoming widely used because it can significantly reduce the time required to conduct pathogen screening tests by eliminating selective enrichment. These methods are sensitive, rapid, technically simple and complement DNA probe, impedance or ELISA methods. Essentially, samples are pre-enriched to increase the population of the target organism. Immunomagnetic beads coated with antibodies specific for the target organism are added to the sample and the organisms of interest are captured by the anti-Salmonella antibody on the surface of the metal bead. A magnet can then be used to attract the metal bead and the Salmonella to the side of the vial. The beads can then be cultured by traditional plating or rapid methods may be used to screen for the presence of Salmonella.
Another means of conducting immunomagnetic separation of bacteria from samples involves continuous circulation of the entire homogenate or rinse sample over a capture area that enhances vortex mixing of the sample. During circulation, the sample is incubated at the target organism’s optimal temperature to promote growth. This approach has been demonstrated to be very effective and rapid for detecting the presence of Salmonella from a variety of food samples.
Chromogenic media also are highly selective and can reduce significantly the cost of confirmatory testing. These tests provide the ability to differentiate Salmonella species, for example, from microorganisms of similar appearance grown on selective culture media, which reduces the number of samples that require further, lengthier testing for identification purposes.
Latex Agglutination. This method tests for the presumptive identification of target bacteria in selective and/or enrichment cultures. The rapid method involves a test reagent comprised of latex particles sensitized with specific antibodies that will react with selected antigens, which is dried onto reaction cards. When an extract of the organism is combined with the test reagent, agglutination occurs, indicating the presence of the organism’s antigen. Detection time is a matter of minutes, following a typical preenrichment step.
Impedance/Conductance. Sophisticated systems have been developed for the rapid detection of microorganisms based on electrical impedance, conductance and capacitance of the medium. As microorganisms grow, they break down relatively uncharged nutrients, such as proteins or fats, into smaller, highly charged molecules like amino acids and fatty acids. Such instruments measure changes in the growth medium at regular intervals and record the time required for sharp and significant changes in the impedance as the detection time (DT) or impedance detection time (IDT). DTs and IDTs are inversely proportional to the initial microbial load in the sample. The IDT and slope of the impedance curves provide valuable information about the initial levels, generation times and growth densities in the sample.
Impedance and conductance systems are computerized, multitasking, multi-user systems that allow electronic data recording and handling, displaying the status of a sample in modes of “accept”or “pass/fail,” as well as trending or tracking of microbiological data. These instruments can be used to detect poor quality or substandard samples in less than eight hours and offer high capacity in terms of simultaneous tests.
DNA Based Methods. DNA hybridization utilizes pathogen-specific DNA probes and a colorimetric detection system for the detection of Salmonella in food samples following culture enrichment. Although each individual DNA hybridization procedure differs slightly, in general, the target bacteria in the sample must be preenriched to increase the number of target organisms in the sample to the point that they can be detected. After preenrichment, hybridization assays are conducted and DNA probes are used to hybridize to adjacent regions on the same target rRNA molecule and capture it for detection by a detector probe treated with a polyclonal anti-fluorescein antibody conjugated to the enzyme horseradish peroxidase (HRP). The complex is reacted with a substrate of HRP, hydrogen peroxide, in the presence of a chromogen. A blue color develops in proportion to the amount of enzyme conjugate bound to the complex and thus, also in proportion to the amount of Salmonella rRNA captured. The reaction is stopped using sulfuric acid that changes the color that has developed from blue to yellow. The color intensity is measured by determining the absorbance at 450nm using a photometer. Absorbance in excess of a predetermined cutoff value indicates a positive result for the presence of the test organism.
Often, results can be obtained in two to four hours following a 20- to 48-hour enrichment period. Direct label probes (DLPs) can reduce the test result time to 1.5 hours, following a 40- to 48-hour enrichment step.
Polymerase chain reaction (PCR) is a another DNA based method used to identify and detect microorganisms of interest to the food industry. PCR amplifies a specific target segment of DNA from a complex mixture of microorganisms as a means of detecting the presence of a particular microorganism. The reaction synthesizes millions of copies of a specific DNA segment in a few hours. The reaction mixture contains a heat-stable DNA polymerase, free nucleotides, and a pair of “primers” (short DNA sequences complementary to the specific target DNA sequence). By amplifying the new target DNA, it becomes possible to detect a specific microbial DNA region by gel electrophoresis or by a computerized DNA detection system. The automated method is highly sensitive and provides very rapid speed to result.
Campylobacter: A Testing Challenge
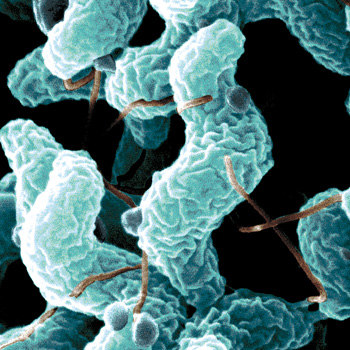
Recognized as the leading microbial cause of foodborne illness, Campylobacter is found in the intestinal tract of many animals, especially birds. As such, the most common food vehicle for Campylobacter jejuni or coli is poultry, pork, and other meats, followed by unpasteurized milk and untreated water. The pathogen also has been associated with mushrooms, clams, cheese, shellfish and eggs. Heat-tolerant, susceptible to freezing and drying, Campylobacter is most frequently transmitted via fecal contamination of skin, meat and milk, through contaminated surface water, and by human shedders. The microaerophilic characteristic of Campylobacter makes conventional methods unwieldy.
Regulation and Research. The National Advisory Committee on Microbiological Criteria for Foods (NACMCF) Campylobacter Subcommittee has been charged by the U.S. Department of Agriculture’s Food Safety and Inspection Service (USDA FSIS) with addressing the analytical utility of Campylobacter identification and quantification methods by:
• Reviewing and comparing the methodologies used for Campylobacter detection in the 1994–1995 and 1999–2000 baseline studies in young chickens;
• Evaluating them for the accuracy and precision that they provide in assessing the prevalence and quantity of Campylobacter on chicken carcasses; and
• Comparing the methodologies used in the two studies with recent methodological advances for their ability to provide data on the presence and quantity of Campylobacter for application in risk assessment and the establishment of baselines.
Thus far, there has been no recommendation to issue a Campylobacter performance standard for poultry and meat products along the lines of the agency’s Salmonella performance standard. A regulation may be slow in coming, since prevalence of Campylobacter in poultry can be fairly high and therefore more challenging to measure than Salmonella prevalence. A more meaningful approach might be to set a baseline standard for the number of Campylobacter per chicken in order to control the number present on the carcass. But until the NACMCF subcommittee completes its review, Campylobacter testing is utilized at the discretion of the processor.
On the research front, USDA Agricultural Research Service (ARS) scientists announced in April 2004 that they had decoded the gene sequence for a specially selected Campylobacter jejuni strain. According to the researchers, this marks the first time a C. jejuni strain from a farm animal—a market chicken—has been sequenced. It is hoped that the identification of the gene code for the C. jejuni strain will lead to the discovery of faster, more reliable ways to detect the microbe in samples from food, as well as animals, humans and water, noted the research team. They also hope the gene-based research will pave the way for simpler, more cost-effective ways of distinguishing look-alike species and strains of Campylobacter for faster identification.
 Methods. As with Salmonella identification and detection techniques, rapid and automated methods developed for Campylobacter include biochemical, immunoassay, immuno-latex agglutination and DNA-based methods (Table 2). Currently, the conventional FDA BAM method requires specialized media, microaerophilic conditions, and a minimum of five days for analysis and up to two weeks for confirmation.
Methods. As with Salmonella identification and detection techniques, rapid and automated methods developed for Campylobacter include biochemical, immunoassay, immuno-latex agglutination and DNA-based methods (Table 2). Currently, the conventional FDA BAM method requires specialized media, microaerophilic conditions, and a minimum of five days for analysis and up to two weeks for confirmation.
FDA scientists now are researching recent molecular technology involving PCR, which can shorten the detection of pathogens to hours instead of days. Their project focuses on the development of the primers and probes for C. jejuni and C. coli and consequent testing for their specificity and sensitivity. The researchers hope to apply the method to several food matrices such as shellfish, dairy and produce.
Next Steps and Selection Tips
Continued research on the part of industry, academic institutions and technology development companies will advance existing bacterial identification and detection methods for Salmonella and Campylobacter in food products. In the meantime, when deciding on the rapid method that is appropriate for a particular company, the processor should consider the type of product manufactured together with speed to result required for that product, cost, and skill level and availability of labor. If the product is extremely perishable and never frozen, time is money and rapid methods are necessary. If the product is of high value, such as breast meat in the U.S., then the need for a same day test increases. If the product is value added, such as fully cooked breast fillets, and will be eaten directly from the package without cooking by a person who may have a vulnerability to food-borne illness, it is extremely important to get results prior to releasing the product for sale. Thus, for this type of product, same-day results are almost a necessity and the added cost of using a same-day assay is well worth it.
On the other hand, if the product is to be frozen and is not perishable, then the company has much more time to gather results and make decisions. It is much less likely that the company would have to be concerned about people consuming the food prior to receiving test results. Also, in the event that the company is testing products in an effort to meet governmental regulations, but the company never detects the bacterium in question, then time is not nearly as important and a longer, less expensive test should be considered. Similarly, if the company tests many samples per day, cost can be a significant issue and must be considered in the cost-benefit analysis. If the processor cannot afford to employ skilled microbiologists, tests that are easy to use and require very little knowledge of microbiology should be selected.
Overall, selection of the right method for a particular company involves balancing the necessity for speed to results, the cost that the company is willing to pay for the test, and the skill level and expense associated with the labor that is available to the company. When taking these factors into account, it much easier to decide between the numerous methods that are available.
Scott M. Russell, Ph.D., is associate professor in the Department of Poultry Science at the University of Georgia, Athens, GA., where he has conducted research and provided extension services to the poultry industry for the past 10 years. His main areas of interest are developing rapid and automated methods for identifying and enumerating pathogenic and spoilage bacteria from foods of animal origin, and identifying methods for eliminating pathogenic and spoilage organisms from poultry during rearing and processing.
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!