Updates from the NoroCORE Project: Progress toward Reducing the Burden of Foodborne Viruses
In a 2014 Food Safety Magazine article,[1] we gave a detailed overview of NoroCORE, the U.S. Department of Agriculture-National Institute of Food and Agriculture (USDA-NIFA) Food Virology Collaborative, in which we outlined the six core functions of the NoroCORE project and plans for what we hoped to accomplish. NoroCORE (the Norovirus Collaborative for Outreach, Research and Education) has continually worked toward its goal of reducing the burden of foodborne viral illness, and we are proud to say we have much to show for our efforts. Now, as we near the end of the grant, we describe some of the Collaborative’s major achievements and long-standing impacts that will continue well beyond the life of the initial project.
What Is Norovirus?
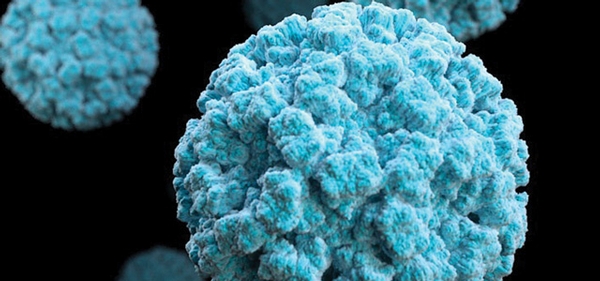
While bacterial causes of foodborne illness, such as pathogenic Escherichia coli and Salmonella, may come first to many people’s minds, noroviruses account for over half of the cases of foodborne illness in the United States, at 5.5 million cases a year.[2] In fact, they are actually the most common cause of acute gastroenteritis in the world.[3] Combining all exposure routes, including foods, norovirus is responsible for about 20 million cases each year in the U.S. alone.[4]
Norovirus has also been called the “perfect human pathogen,” because it is highly contagious, is shed in high numbers by infected individuals, evolves rapidly and seems adept at avoiding our ability to create lasting immunity.[5] This last trait, coupled with the fact that most of us recover from norovirus infections, means that on average, we will experience norovirus five times during the course of our lives.[2] Add the fact that it is a very hardy virus that is resistant to most disinfectants and sanitizers when used as directed by their manufacturers, and it’s clear why this pathogen is a big problem around the world. It is a major concern for several industries, but foodservice has a particular interest, as most foodborne norovirus outbreaks occur in restaurants or similar establishments.[6]
NoroCORE Tackles the Problem Holistically
Realizing that a complex problem often requires a creative and multifaceted solution, USDA-NIFA funded the NoroCORE project[7] with a $25 million Coordinated Agricultural Project grant in 2011. The purpose of the project has been to increase our scientific knowledge of foodborne viruses, particularly norovirus, and then communicate and translate this information into real-world applications that will reduce the burden of disease associated with these viruses. NoroCORE has successfully brought researchers and resources from varied scientific disciplines together, while also providing strong education and outreach programs to a diverse stakeholder group.
In just a few short years, NoroCORE has grown from 18 collaborating institutions to 25 and includes 36 principal investigators. We also have a varied stakeholder group, hailing from regulatory and public health agencies, food safety organizations and industries such as food production and processing, foodservice and retail, diagnostics and testing, sanitation and hygiene and the cruise line industry. This equates to over 200 individuals representing over 60 entities. In addition to bringing an even greater wealth of knowledge and experience to the project, interaction with our stakeholder group helps ensure that the research can be more readily implemented for the benefit of public health.
Success Stories from NoroCORE
NoroCORE has made real and substantial strides in solving a very complex problem. Here are a few of our success stories.
1. The cultivation of human norovirus[8]
One of the classic ways scientists work with viruses is to expose them to living cells, typically of animal origin, in culture, allowing them to infect and multiply within those cells. This allows us to better understand viral biology; evaluate the efficacy of candidate disinfection strategies; and develop methods to more easily detect them. While we can culture many other viruses (including some viruses from the same family), researchers had tried unsuccessfully to culture human norovirus since we first learned of its existence almost 50 years ago. Not surprisingly, this lack of a culture system has long been considered the most significant barrier to norovirus research.[9]
The systematic examination of the merits of so-called human norovirus surrogates has been an important objective of NoroCORE’s Molecular Virology Core. Team members have produced much data confirming the selection of the “best” cultivable surrogate to be very dependent upon the conditions or treatments being tested. This means there is no “silver bullet” when it comes to using a cultivable replacement in human norovirus studies. That said, NoroCORE has also sponsored work under the direction of Dr. Mary Estes at Baylor College of Medicine (BCM) to develop a human norovirus culture system. The BCM group was successful, using three-dimensional structures of human intestinal cells to grow human norovirus.[9,10] The method has been reproduced in other labs, and scientists all over the world are embarking on training. Although still in its infancy, this method promises to be the start of a new era in norovirus research, both basic and applied.
2. Outreach to relevant commodity groups
NoroCORE meets the traditional definition of extension and outreach by communicating with fresh produce farmers, shellfish harvesters and food production and service groups at conferences, as well as on the farm or dock. In this regard, the NoroCORE team has worked closely with the Interstate Shellfish Sanitation Conference (ISSC)[11] to establish a multi-tiered approach for disseminating information about viral contamination risks associated with consumption of raw or undercooked shellfish. The focus has been on the prevention of human sewage contamination in shellfish-harvesting waters, as this is believed to be the most common means by which molluscan shellfish become contaminated with norovirus.[12] For instance, NoroCORE and ISSC jointly sponsored a conference on preventing fecal contamination of harvesting waters through the use of alternative microbial indicators, updated a DVD focusing on overboard waste dumping and waste management for boats and surveyed recreational boaters and fishermen to understand the best means of reaching these groups. This last effort evolved into an interactive exhibit called “Don’t Poo (or Spew) in the Blue” that is being presented at a series of eight boat shows in the U.S. (Figure 1).
 Other examples of commodity-specific outreach include fact sheets[13] and the development of customizable vomiting and fecal matter cleanup guidelines for use in foodservice facilities. NoroCORE has also worked closely with the Produce Safety Alliance (PSA) to provide virus-specific information that has been integrated into the PSA national regulatory training curriculum required by the Food Safety Modernization Act’s Produce rule.
Other examples of commodity-specific outreach include fact sheets[13] and the development of customizable vomiting and fecal matter cleanup guidelines for use in foodservice facilities. NoroCORE has also worked closely with the Produce Safety Alliance (PSA) to provide virus-specific information that has been integrated into the PSA national regulatory training curriculum required by the Food Safety Modernization Act’s Produce rule.
3. NorOPTIMAL
How great would it be if we could predict what would happen in a specific facility when norovirus was introduced? What if we could even go back in time and see what actions would have prevented a norovirus outbreak, or go forward in time and see what might be the best means of containing it? That is exactly what NorOPTIMAL was created to do.
NorOPTIMAL, or the Norovirus On-line Predictive Tool to Investigate Mitigation Alternatives, is a quantitative risk-modeling program that can predict the effects of different parameters in a spatial system. It has been tailored to norovirus, and wherever possible, the parameters are based in scientific data. For example, how much norovirus is transferred to a surface by a tactile event? What is the efficacy of different disinfectants? How much virus is dispersed when someone vomits in a room?
The model is built so that the user can simulate a specific environment (e.g., maps of the facility), identify one or more contamination events and then track norovirus as it spreads in time and space. Even the actions of individuals in the facility and the objects in the rooms can be manipulated. Once the parameters are set, the probabilistic model is run over and over to give the most likely outcomes. The impact of different control strategies (e.g., increased handwashing compliance, better disinfection, removal of ill individuals) on those outcomes can also be simulated. The prototype model has been produced for extended-care health facilities but is being adapted for use by the foodservice industry. This powerful tool can provide a wealth of useful information, such as the identity of hot spots in the facility that should receive extra attention when cleaning, the estimated financial costs of different interventions and a prediction of how long an outbreak will last before it is contained.
4. Estimates of disease burden
 NoroCORE provided some of the funding that has led to a more comprehensive understanding of the burden of norovirus illness in the U.S. This work, done by our U.S. Centers for Disease Control and Prevention (CDC) collaborators, includes better information on the importance of foods in transmission of norovirus and attribution of disease to specific foods and settings (Figure 2). For example, while cruise ships are often maligned as a common source of norovirus outbreaks, fewer than 0.5 percent of cruises experience an outbreak, amounting to only 0.01 percent of the nation’s total norovirus cases.[14] By comparison, there is, on average, one foodborne norovirus outbreak reported every day in the U.S.[15] Foodborne transmission accounts for about a quarter of all norovirus cases, and in the last couple of years, it was affirmed that a majority of these foodborne events occur in restaurants and foodservice. Looking deeper, 70 percent of the time, the contamination can be traced back to an infected worker who, more often than not, had bare-hand contact with food and/or did not practice good hand hygiene.[6] This tells us that to have the greatest impact on public health, we should be more focused on controlling the means by which norovirus reaches our retail food supply and preventing ill workers from coming into contact with food.
NoroCORE provided some of the funding that has led to a more comprehensive understanding of the burden of norovirus illness in the U.S. This work, done by our U.S. Centers for Disease Control and Prevention (CDC) collaborators, includes better information on the importance of foods in transmission of norovirus and attribution of disease to specific foods and settings (Figure 2). For example, while cruise ships are often maligned as a common source of norovirus outbreaks, fewer than 0.5 percent of cruises experience an outbreak, amounting to only 0.01 percent of the nation’s total norovirus cases.[14] By comparison, there is, on average, one foodborne norovirus outbreak reported every day in the U.S.[15] Foodborne transmission accounts for about a quarter of all norovirus cases, and in the last couple of years, it was affirmed that a majority of these foodborne events occur in restaurants and foodservice. Looking deeper, 70 percent of the time, the contamination can be traced back to an infected worker who, more often than not, had bare-hand contact with food and/or did not practice good hand hygiene.[6] This tells us that to have the greatest impact on public health, we should be more focused on controlling the means by which norovirus reaches our retail food supply and preventing ill workers from coming into contact with food.
Looking ahead, we will continue to work with CDC and other colleagues at Emory University to better characterize disease burden in at-risk human populations (e.g., the very young and the elderly) and the health implications of asymptomatic norovirus infections.
5. How the heck do we inactivate norovirus?
 While preventing norovirus contamination is the best control measure, sometimes it just happens. This means that we must also build into the food system some means to inactivate the virus if it is there. Because of work done by the NoroCORE team, we know much more about how the virus is spread and how difficult it is to “kill.” For instance, investigators at North Carolina State University (NCSU) created a vomiting machine (Figure 3) to understand whether the virus is aerosolized when someone vomits and, if so, how much.[16] The answer is that a very tiny amount of virus is released into the air after a simulated vomiting event, but it would be enough to cause human disease. Coupled with the fact that the aerosol spreads over several feet, these data suggest that wide areas need to be disinfected after a vomiting event.
While preventing norovirus contamination is the best control measure, sometimes it just happens. This means that we must also build into the food system some means to inactivate the virus if it is there. Because of work done by the NoroCORE team, we know much more about how the virus is spread and how difficult it is to “kill.” For instance, investigators at North Carolina State University (NCSU) created a vomiting machine (Figure 3) to understand whether the virus is aerosolized when someone vomits and, if so, how much.[16] The answer is that a very tiny amount of virus is released into the air after a simulated vomiting event, but it would be enough to cause human disease. Coupled with the fact that the aerosol spreads over several feet, these data suggest that wide areas need to be disinfected after a vomiting event.
We have also confirmed the long-suspected hypothesis that commonly used alcohol-based hand sanitizers cannot be relied upon to completely inactivate norovirus. Yes, as your mama said, handwashing remains the best control. Right now, NoroCORE investigators are comprehensively evaluating commercial and emerging surface disinfectants for anti-human noroviral efficacy. Keeping in mind that as we do not yet have a readily available, simple cell culture propagation method for human norovirus, it is difficult to determine just how effective a disinfectant might be. However, using a series of molecular and microscopic techniques, we can get a good idea. While it is too early for global conclusions, most products tested show some efficacy but often not the 4-log inactivation necessary to make U.S. Environmental Protection Agency-approved label claims. Chlorine at high concentrations does work but is fraught with its own problems. There is no ideal solution, but we are slowly narrowing down components that, when used in combination, might provide products with greater efficacy, less toxicity and less corrosivity.
6. Capacity building on multiple levels
NoroCORE has defined capacity building to include tangible products, such as new technologies and materials, as well as intangible ones, such as supporting those inside the Collaborative with a network of experts. Working in a specific field requires specific materials, some of which are so new or unique that they cannot be purchased from a catalog. To date, our reagent exchange program has documented over 150 exchanges among researchers affiliated with the Collaborative. This exchange has greatly expanded research capacity and facilitated cross-disciplinary collaboration. As for scholarly enrichment, there are over 3,200 articles in our literature database,[17] the abstracts of which are archived and publicly available on our website. Our investigators have mentored over 50 graduate students through NoroCORE-funded research projects and fellowships, as well as 15 BRITE (Biomanufacturing Research Institute and Technology Enterprise) summer internships through our collaboration with North Carolina Central University. Training these young people will enrich and shape the field for years to come.
NoroCORE also serves the scientific community at large. For example, at the 2016 International Association for Food Protection annual meeting, several NoroCORE senior investigators gave a two-day workshop on foodborne virus detection methods. We also recently added a web page with teaching materials[18] for use by educators and the
public.
7. Public outreach and engagement
 Six years ago, the general public was not very familiar with the term “norovirus,” although people were very familiar with the disease it causes. NoroCORE is proud to have been part of the public conversation to bring about greater understanding of norovirus. Our general approach has been to use social media as a tool to educate and interact with consumers and professionals, and in just a couple of years, our posts and campaigns have had over 110,000 views and led to over 4,000 engagements. New discoveries, helpful information and a little humor have been the backbone of our campaigns (Figure 4), and we’ve found that people like to share their stories[19] about norovirus (often in impressive and hilarious detail) and want to know how to protect themselves and their families. We even have a cheeky norovirus particle named Naughty Noro[20] that tweets at people who are talking about their norovirus infections or current outbreaks, sparking conversations about what not to do (since of course he wants to keep spreading).
Six years ago, the general public was not very familiar with the term “norovirus,” although people were very familiar with the disease it causes. NoroCORE is proud to have been part of the public conversation to bring about greater understanding of norovirus. Our general approach has been to use social media as a tool to educate and interact with consumers and professionals, and in just a couple of years, our posts and campaigns have had over 110,000 views and led to over 4,000 engagements. New discoveries, helpful information and a little humor have been the backbone of our campaigns (Figure 4), and we’ve found that people like to share their stories[19] about norovirus (often in impressive and hilarious detail) and want to know how to protect themselves and their families. We even have a cheeky norovirus particle named Naughty Noro[20] that tweets at people who are talking about their norovirus infections or current outbreaks, sparking conversations about what not to do (since of course he wants to keep spreading).
We have also had success with citizen science events, such as a mock norovirus outbreak[21] at the 2015 International Association for Food Protection meeting. We recently launched another citizen science exercise on the importance of handwashing as illustrated by pictures of “Employees must wash hands” signs in restaurant bathrooms, voluntarily submitted by participants.[22] As much as possible, we try to make our communications educational as well as fun, sharing information that will help people make informed decisions about food safety and norovirus prevention.
Conclusion
USDA-NIFA made a big gamble when they embraced the team science approach and funded a project as massive as NoroCORE. We believe that NoroCORE’s structure, with six interconnected core areas[23] covering the functions of research, extension and education, along with public and stakeholder engagement, has been a good model for this particular approach to scientific problem solving. The NoroCORE program is currently being evaluated by an external group, which will allow us to identify what worked, what didn’t work and what components are critical to a large collaborative such as this one. But while our outputs follow the classic metrics of research papers, intellectual property, knowledge exchange and education, the outcomes of the project will continue to be realized in real-world applications. We hope that those will be greater awareness of the burden of norovirus illness, improved prevention and control strategies, methods that move the science forward and a reduction in disease burden. We look forward to seeing our efforts continue to mature into the future.
Elizabeth Bradshaw, D.V.M., M.P.H., is the Extension Associate for NoroCORE at NCSU. She has a background in science communication and epidemiology.
Otto D. Simmons III, Ph.D., is an Area-Specialized Agent in Food Safety in the Department of Horticultural Science at NCSU and previously worked as a research assisant professor and Extension Specialist for NoroCORE. His background is in public health and environmental microbiology, and his goal is to provide practical information to targeted stakeholder groups to prevent foodborne illness.
Lee-Ann Jaykus, Ph.D., is William Neal Reynolds Distinguished Professor in the Department of Food, Bioprocessing and Nutrition Sciences at NCSU. Her current research efforts are varied and focus on food virology, development of molecular methods for foodborne pathogen detection, application of quantitative risk assessment in food safety and understanding the ecology of pathogens in foods.
References
1. www.food-safety.com/magazine-archive1/junejuly-2014/food-virology-collaborative-norocore-tackles-foodborne-viruses/.
2. Scallan, E et al. 2011. “Foodborne Illness Acquired in the United States – Major Pathogens.” Emerg Infect Dis 17:7–15.
3. Lopman, BA et al. 2016. “The Vast and Varied Global Burden of Norovirus: Prospects for Prevention and Control.” PLoS Med 13, e1001999.
4. Hall, AJ et al. 2013. “Norovirus Disease in the United States.” Emerg Infect Dis 19:1198–1205.
5. Hall, AJ. 2012. “Noroviruses: The Perfect Human Pathogens?” J Infect Dis 205:1622–1624.
6. Hall, AJ et al. 2014. “Vital Signs: Foodborne Norovirus Outbreaks – United States, 2009–2012.” MMWR 63:491–495.
7. norocore.ncsu.edu/.
8. norocore.ncsu.edu/download/5837/.
9. Ettayebi, K et al. 2016. “Replication of Human Noroviruses in Stem Cell-Derived Human Enteroids.” Science 353:1387–1393.
10. norocore.ncsu.edu/a-historic-moment-in-virology-the-cultivation-of-human-norovirus.
11. www.issc.org/.
12. Campos, CJA and DN Lees. 2014. “Environmental Transmission of Human Noroviruses in Shellfish Waters.” Appl Environ Microbiol 80:3552–3561.
13. norocore.ncsu.edu/resources/factsheets-infographics/
14. Freeland, AL et al. 2016. “Acute Gastroenteritis on Cruise Ships – United States, 2008–2014.” MMWR 65:1–5.
15. Hall, AJ et al. 2012. “Epidemiology of Foodborne Norovirus Outbreaks, United States, 2001–2008.” Emerg Infect Dis 18:1566–1573.
16. Tung-Thompson, G et al. 2015. “Aerosolization of a Human Norovirus Surrogate, Bacteriophage MS2, during Simulated Vomiting.” PLoS One 10, e0134277.
17. norocorelit.com/.
18. norocore.ncsu.edu/resources/educational-materials/.
19. norocore.ncsu.edu/category/all/page/2/.
20. twitter.com/NaughtyNoro.
21. norocore.ncsu.edu/about/meetings-events/2015-iafp-stakeholder-reception-exhibit-and-presentations/.
22. www.pinterest.com/norocoreusdanif.
23. norocore.ncsu.edu/about/overview/.
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!